Fill Your Tb Test Form
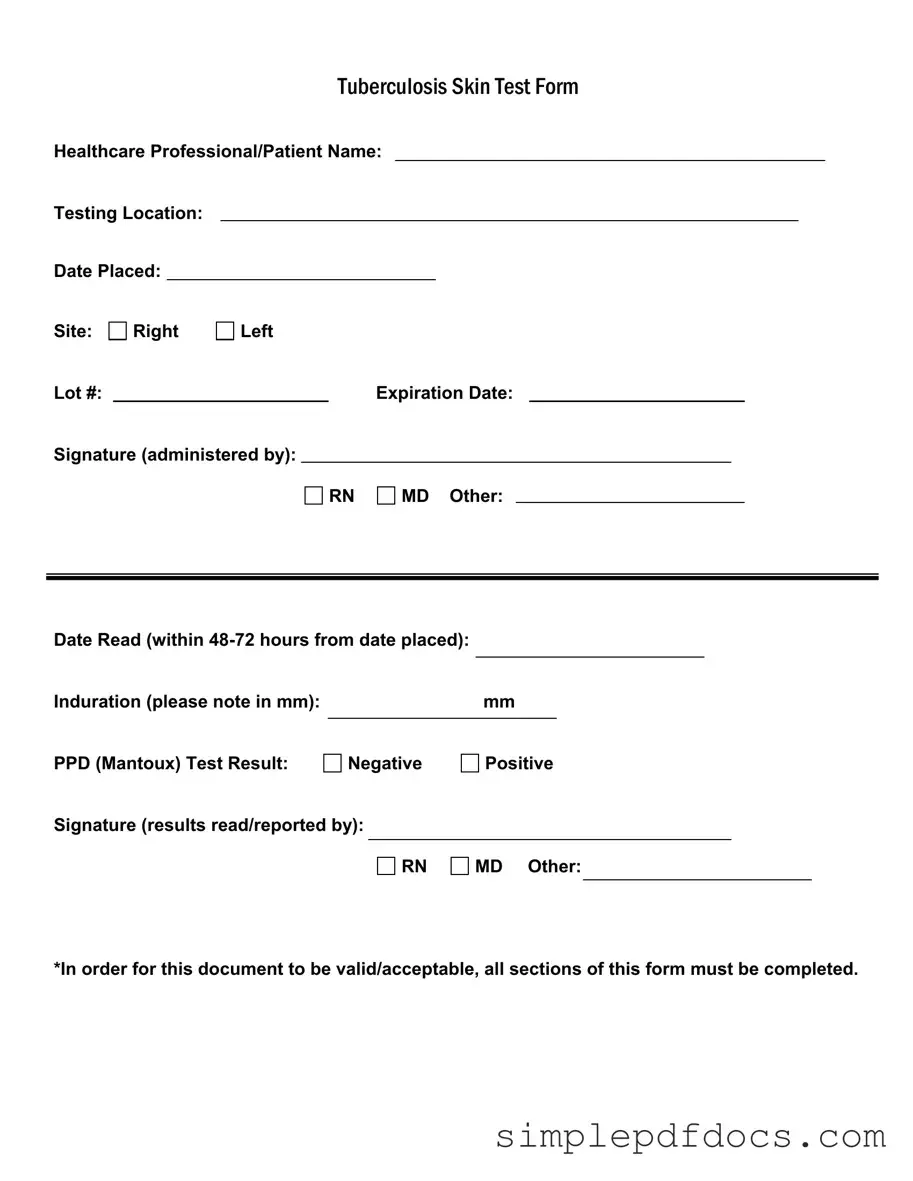
The Tuberculosis (TB) Skin Test Form serves as a crucial document in the screening process for tuberculosis, a contagious bacterial infection that primarily affects the lungs. This form requires detailed information from both the healthcare professional and the patient, ensuring a comprehensive record of the testing process. Key elements include the names of the healthcare professional and patient, the testing location, and the date the test was placed. Additionally, the form specifies the site of the test, whether on the right or left arm, along with the lot number and expiration date of the test material. The signature of the administering professional—be it a registered nurse, medical doctor, or other qualified personnel—validates the administration of the test. It is essential to read the results within 48 to 72 hours, noting the induration measurement in millimeters, which indicates the body's reaction to the test. The final section captures the test result, categorized as either negative or positive, and requires the signature of the professional who interpreted the results. For the document to be considered valid and acceptable, all sections must be meticulously completed, underscoring the importance of accuracy in tuberculosis screening.
More PDF Templates
2b Mindset Tracker Spiral - Enjoy the process with a flexible mindset towards food.
To ensure a successful transfer of ownership, it's vital to use the proper documentation. This is where the importance of the RV Bill of Sale comes into play. For a thorough understanding of this process, refer to the guide on the essential RV Bill of Sale requirements found here.
Texas Driver License Renewal Form - The form provides a pathway to check for outstanding vehicle-related fees.
Document Specifics
| Fact Name | Description |
|---|---|
| Form Purpose | The Tuberculosis Skin Test Form is used to document the administration and results of the PPD (Mantoux) test. |
| Healthcare Professional Requirement | The form must be completed and signed by a qualified healthcare professional, such as an RN or MD. |
| Testing Location | The location where the test is administered must be clearly indicated on the form. |
| Timing for Reading | The results of the test must be read within 48 to 72 hours after placement for accuracy. |
| Induration Measurement | The induration, or swelling, must be measured in millimeters and recorded on the form. |
| Result Documentation | Test results must be noted as either negative or positive, and signed by the healthcare professional who read the results. |
| Completion Requirement | All sections of the form must be fully completed for it to be considered valid and acceptable. |
| State-Specific Regulations | In some states, specific laws govern the use of this form, including documentation requirements under public health statutes. |
How to Write Tb Test
Completing the TB Test form is an essential step in documenting your test results accurately. Once you have filled out the form, it will serve as an official record of your tuberculosis skin test, which is crucial for various health-related purposes. Follow the steps below to ensure you complete the form correctly.
- Begin by entering the name of the healthcare professional or patient at the top of the form.
- Next, indicate the testing location where the TB test is administered.
- Fill in the date when the test was placed.
- Specify the site of the test by marking either the right or left side.
- Record the lot number of the PPD (Mantoux) used for the test.
- Enter the expiration date of the PPD.
- Have the healthcare professional administering the test sign the form, indicating their title (RN, MD, or other).
- After 48-72 hours, return to have the test read. Fill in the date when the results are read.
- Measure the induration in millimeters and note this value on the form.
- Mark the PPD test result as either negative or positive.
- Finally, the healthcare professional who reads the results should sign the form, again indicating their title (RN, MD, or other).
Make sure to review the completed form for accuracy. All sections must be filled out for the document to be valid and acceptable.
Dos and Don'ts
When filling out the TB Test form, attention to detail is crucial. Here are some important dos and don’ts to ensure accuracy and compliance.
- Do ensure that all sections of the form are completed. Missing information can lead to delays.
- Do double-check the testing location and date placed. This information is vital for record-keeping.
- Do accurately note the induration measurement in millimeters. This is essential for interpreting results.
- Do have the form signed by the healthcare professional administering the test. This validates the procedure.
- Don't leave any fields blank. Incomplete forms may be deemed invalid.
- Don't forget to record the expiration date of the lot number. This ensures the test's reliability.
- Don't ignore the time frame for reading the results. Results must be read within 48-72 hours.
By following these guidelines, you can help ensure that the TB Test form is filled out correctly and efficiently.
Documents used along the form
The Tuberculosis (TB) Test form is essential for documenting the results of a TB skin test, but several other documents often accompany it in healthcare settings. These forms help ensure comprehensive patient care and compliance with health regulations. Below is a list of common forms used alongside the TB Test form.
- Patient Consent Form: This document confirms that the patient has been informed about the TB test and agrees to undergo the procedure. It protects the healthcare provider by ensuring that the patient understands the purpose and potential risks involved.
- Medical History Form: A detailed account of a patient’s medical background, this form helps healthcare providers assess any previous TB exposure, existing health conditions, or allergies that could affect test results or treatment.
- Sales Tax Form: The Florida Forms are essential for completing the Sales and Use Tax Return (DR-15CS), which is required for reporting sales tax obligations in Florida.
- Vaccination Record: This form lists all vaccinations a patient has received. It is important for determining if a patient has received the BCG vaccine, which can affect the interpretation of TB test results.
- Follow-Up Care Plan: After the TB test, a follow-up care plan outlines any additional testing or treatment required based on the results. It ensures that patients receive timely care if they test positive.
- Referral Form: If a patient requires further evaluation by a specialist, a referral form is used to direct them to the appropriate healthcare provider. This document facilitates continuity of care.
- Results Notification Form: This form is used to communicate the results of the TB test to the patient. It includes important information about next steps and any necessary follow-up actions.
- Insurance Authorization Form: If applicable, this document is needed to obtain approval from the patient’s insurance provider for the TB test. It ensures that the costs are covered, easing financial concerns for the patient.
These documents work together to create a comprehensive approach to TB testing and management. Ensuring that all necessary forms are completed and submitted helps maintain a high standard of patient care and compliance with health regulations.