Fill Your Progress Notes Form
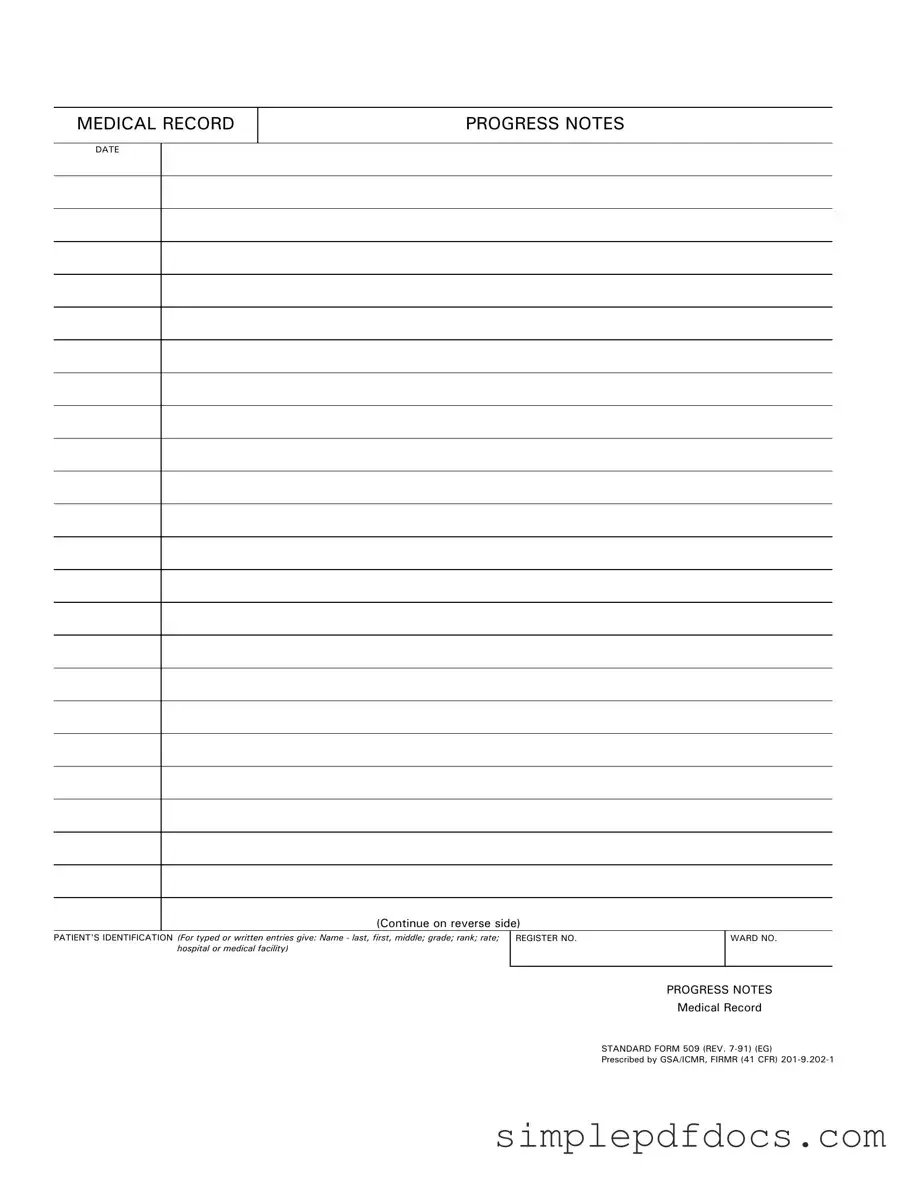
In the realm of healthcare documentation, the Progress Notes form serves as a vital tool for recording patient information and treatment updates. This form, officially designated as Standard Form 509, is a structured document that captures essential details about a patient's visit or ongoing care. It includes key elements such as the patient's identification, which requires comprehensive information like the patient's name, grade, rank, rate, and the medical facility where they are being treated. The date of entry is prominently featured, ensuring that all notes are time-stamped for accurate tracking of the patient's medical history. Additionally, the form allows for the continuation of notes on the reverse side, accommodating the need for thorough documentation. By adhering to these standardized guidelines, healthcare professionals can maintain clear and organized records, ultimately enhancing patient care and communication within medical teams.
More PDF Templates
Printable Return to Work Doctors Note - The Work Release form can encourage collaboration between correctional facilities and local businesses.
For couples eager to embark on their journey of marriage, completing the Florida Marriage Application form is vital. This application not only marks the beginning of the marriage license process, valid for just 60 days, but also requires couples to familiarize themselves with the specific requirements involved. To ensure all necessary steps are appropriately followed, refer to the detailed instructions provided at Florida Forms, which can help facilitate a smooth wedding planning experience.
How to Write a Continuance Letter for Court - Fill in the required details clearly and accurately.
Bol Generator - It also includes information about the freight charges associated with the shipment.
Document Specifics
| Fact Name | Details |
|---|---|
| Form Purpose | The Progress Notes form is used to document a patient's medical history and ongoing treatment in a structured manner. |
| Governing Authority | This form is prescribed by the General Services Administration (GSA) and is governed by the Federal Information Resources Management Regulation (FIRMR). |
| Standardization | Standard Form 509 is a standardized document, ensuring consistency in medical record-keeping across various facilities. |
| Revision History | The current version of the form is Standard Form 509 (REV. 7-91), indicating it was last revised in July 1991. |
| Patient Identification | The form requires detailed patient identification, including name, grade, rank, rate, and the medical facility where treatment is provided. |
| Record Keeping | Progress Notes are essential for maintaining accurate medical records, which can be crucial for ongoing patient care. |
| Legal Compliance | Using this form helps ensure compliance with federal regulations regarding medical documentation and patient confidentiality. |
| Continuation Option | There is an option to continue notes on the reverse side of the form, allowing for additional space when necessary. |
| Usage Across Facilities | This form is utilized across various medical facilities, including hospitals and clinics, to maintain uniformity in patient records. |
How to Write Progress Notes
Filling out the Progress Notes form is an important task that helps ensure accurate medical documentation. By carefully following these steps, you can complete the form efficiently and effectively.
- Start by entering the date at the top of the form. This should reflect the date of the patient visit or the date of the notes being made.
- Next, fill in the patient's identification section. Include the patient's last name, first name, and middle initial. Additionally, provide their grade, rank, and rate, if applicable. Don’t forget to include the name of the hospital or medical facility.
- Locate the register number field and enter the patient's unique identification number. This helps in tracking and managing patient records.
- In the ward number section, specify the ward where the patient is located. This is crucial for ensuring that the notes are associated with the correct area of the facility.
- Finally, proceed to the progress notes section. Here, document any relevant observations, treatments, or changes in the patient's condition. Make sure to write clearly and concisely.
Once you have completed these steps, review the form for accuracy. Double-check that all required fields are filled out and that the information is correct. This will help maintain the integrity of the patient's medical record.
Dos and Don'ts
When filling out the Progress Notes form, it’s important to ensure accuracy and clarity. Here’s a list of things to keep in mind:
- Do include the patient's full name, including last, first, and middle names.
- Do provide the patient's grade, rank, and rate accurately.
- Do ensure the date is clearly marked at the top of the form.
- Do use clear and concise language when writing notes.
- Don’t leave any sections blank; if a section is not applicable, indicate that clearly.
- Don’t use abbreviations that may not be universally understood.
- Don’t write in a manner that could be misinterpreted; clarity is key.
- Don’t forget to sign and date the form after completion.
Documents used along the form
The Progress Notes form is an essential document in medical records, capturing a patient's ongoing treatment and progress. Several other forms complement this document, ensuring comprehensive patient care and accurate record-keeping. Below is a list of these important forms and documents.
- Admission Assessment Form: This form collects initial information about the patient upon admission, including medical history, current medications, and allergies.
- Discharge Summary: Summarizes the patient's treatment and progress during their stay, providing essential information for follow-up care after leaving the facility.
- Medication Administration Record (MAR): Tracks all medications given to the patient, including dosages and administration times, ensuring proper medication management.
- Care Plan: Outlines the patient's treatment goals and interventions, serving as a roadmap for healthcare providers during the patient's care.
- Residential Lease Agreement: For accurate documentation of rental agreements, refer to the comprehensive Residential Lease Agreement guidelines to secure your rights as a tenant or landlord.
- Referral Form: Used when a healthcare provider refers a patient to a specialist, including pertinent medical history and reasons for the referral.
- Informed Consent Form: Documents that a patient understands and agrees to a proposed treatment or procedure, ensuring legal protection for both the patient and provider.
- Patient History Form: Gathers comprehensive background information on the patient, including past illnesses, surgeries, and family medical history.
- Vital Signs Record: Tracks the patient's vital signs over time, including temperature, pulse, respiration, and blood pressure, which are crucial for monitoring health status.
These forms work together to create a complete picture of a patient's health journey. Proper documentation is vital for effective communication among healthcare providers and for delivering high-quality patient care.