Attorney-Approved Do Not Resuscitate Order Form
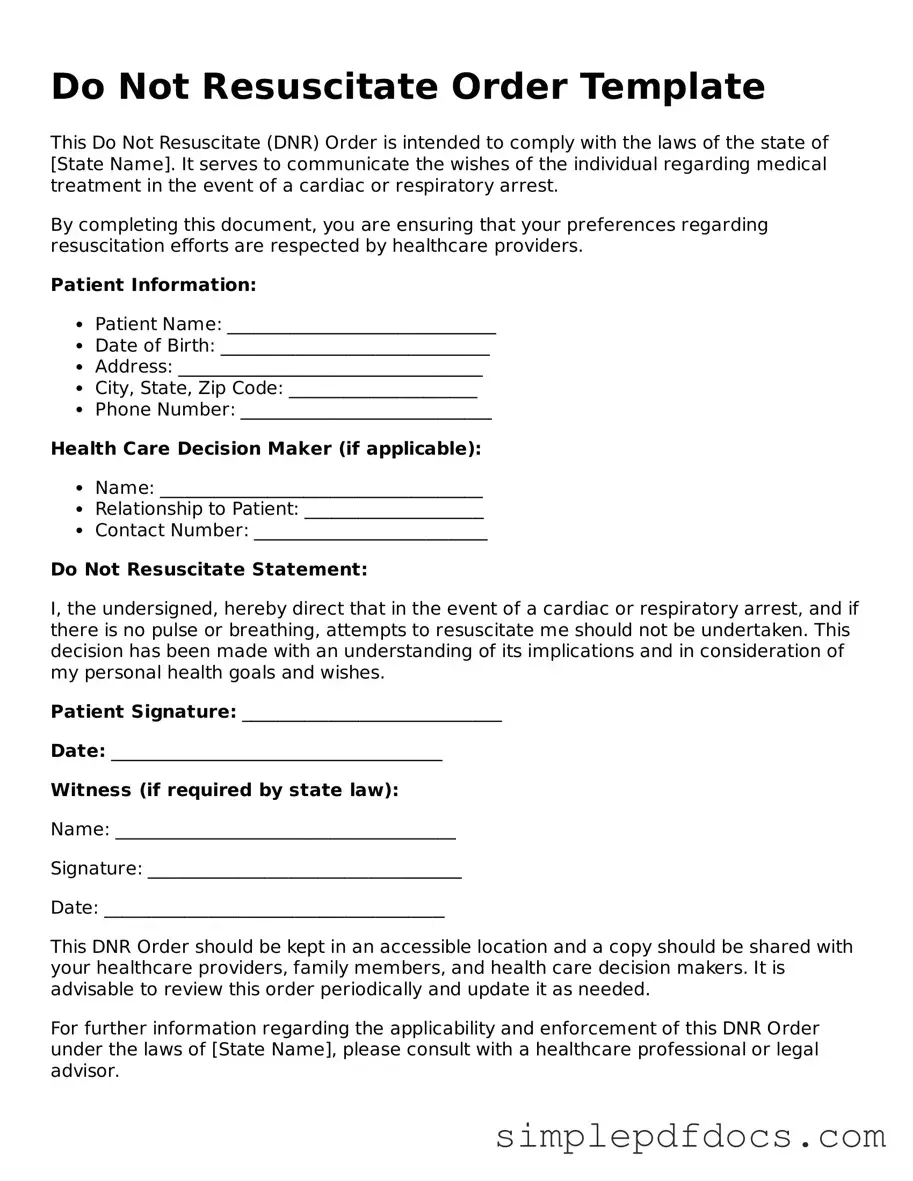
The Do Not Resuscitate (DNR) Order form is a crucial document that allows individuals to express their wishes regarding medical treatment in the event of a life-threatening situation. This form typically includes essential information such as the patient's name, date of birth, and medical history. It serves as a clear directive to healthcare providers, indicating that the patient does not wish to receive cardiopulmonary resuscitation (CPR) or other life-sustaining measures if their heart stops beating or if they stop breathing. In addition to outlining the patient's preferences, the DNR Order often requires signatures from both the patient and a physician, ensuring that the decision is made thoughtfully and in consultation with a medical professional. Understanding the implications of a DNR Order is vital for patients and their families, as it can significantly impact end-of-life care and the quality of life during critical moments. By facilitating open discussions about personal values and medical wishes, this form empowers individuals to take control of their healthcare decisions, providing peace of mind for both patients and their loved ones.
State-specific Do Not Resuscitate Order Forms
Check out Other Documents
Garage Rental Agreement - It may specify any modifications that tenants can or cannot make to the property.
To understand the importance of the FR-44 Florida form, it's essential for drivers to familiarize themselves with the requirements outlined in the state's Financial Responsibility Law; resources like Florida Forms can provide valuable information on how to properly complete this document.
How to Become a Professional Cuddler - Cuddling can be a therapeutic experience; join us to explore this option.
PDF Details
| Fact Name | Description |
|---|---|
| Definition | A Do Not Resuscitate (DNR) order is a legal document that prevents medical personnel from performing cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Purpose | The primary purpose of a DNR order is to respect the wishes of individuals who do not wish to undergo aggressive resuscitation efforts. |
| Legal Status | DNR orders are recognized in all 50 states, but the specific requirements and forms can vary by state. |
| State-Specific Forms | Each state has its own DNR form. For example, in California, the DNR form is governed by the California Health and Safety Code, Section 7180. |
| Signature Requirements | Most states require the DNR order to be signed by the patient or their legal representative, as well as a physician. |
| Emergency Medical Services (EMS) | EMS personnel are trained to recognize and honor DNR orders, provided they are properly documented and visible at the time of an emergency. |
| Revocation | A DNR order can be revoked at any time by the patient or their legal representative, and this should be communicated clearly to healthcare providers. |
How to Write Do Not Resuscitate Order
Filling out a Do Not Resuscitate Order (DNR) form is an important step in expressing your healthcare preferences. This document allows you to communicate your wishes regarding resuscitation efforts in case of a medical emergency. Follow these steps to complete the form accurately.
- Obtain the DNR form from your healthcare provider or download it from a reliable source.
- Read the form carefully to understand all sections and requirements.
- Fill in your full name, date of birth, and any other personal information requested.
- Indicate your wishes regarding resuscitation by checking the appropriate box. This may include options for full resuscitation or no resuscitation.
- Consult with your healthcare provider to discuss your choices and ensure they align with your medical condition and goals.
- Sign and date the form in the designated area to validate your wishes.
- Have a witness sign the form if required. This may be a healthcare professional or another adult, depending on your state’s regulations.
- Make copies of the completed form for your records and share them with your healthcare provider, family members, and anyone else involved in your care.
Once you have completed the form, ensure it is stored in a safe place where it can be easily accessed by your healthcare team. Regularly review and update the document as needed, especially if your health status or preferences change.
Dos and Don'ts
When filling out a Do Not Resuscitate (DNR) Order form, it is crucial to approach the task with care and consideration. This document can significantly impact medical care and end-of-life decisions. Here are ten things to keep in mind:
- Do discuss your wishes with your healthcare provider. Open communication ensures that your preferences are understood.
- Do involve family members in the conversation. Their support and understanding can be vital.
- Do ensure that the form is filled out completely. Incomplete forms may lead to confusion in critical situations.
- Do keep a copy of the signed DNR Order in a visible place. Accessibility is key when emergencies arise.
- Do review and update the form as necessary. Life circumstances and preferences may change over time.
- Don’t rush the process. Take your time to reflect on your choices and their implications.
- Don’t assume that verbal agreements are sufficient. Written documentation is essential for clarity.
- Don’t overlook the importance of understanding the implications of a DNR Order. Make sure you fully grasp what it entails.
- Don’t forget to discuss your DNR Order with all healthcare providers involved in your care. Consistency is important.
- Don’t ignore local laws and regulations regarding DNR Orders. They can vary significantly by state.
By following these guidelines, individuals can ensure that their DNR Orders accurately reflect their wishes and provide clarity for their loved ones and healthcare providers.
Documents used along the form
A Do Not Resuscitate (DNR) Order is a crucial document that outlines a person's wishes regarding resuscitation efforts in the event of a medical emergency. However, several other forms and documents may complement a DNR Order, ensuring that an individual's healthcare preferences are clearly communicated and respected. Below is a list of these essential documents.
- Advance Healthcare Directive: This document allows individuals to specify their healthcare preferences in advance, including decisions about medical treatment and end-of-life care.
- Durable Power of Attorney for Healthcare: This legal document appoints someone to make healthcare decisions on behalf of an individual if they become unable to do so themselves.
- Living Will: A living will outlines specific medical treatments an individual wishes to receive or avoid, particularly in terminal or irreversible conditions.
- Physician Orders for Life-Sustaining Treatment (POLST): This form translates a patient's wishes into actionable medical orders, ensuring that healthcare providers follow those wishes during emergencies.
- Do Not Intubate (DNI) Order: This document specifically instructs medical personnel not to insert a breathing tube, often used alongside a DNR Order.
- Healthcare Proxy: Similar to a durable power of attorney, this document designates a person to make medical decisions for someone who cannot communicate their wishes.
- Organ Donation Consent: This form expresses an individual's wishes regarding organ donation after death, providing clarity to family and healthcare providers.
- Medical History Record: A comprehensive record of an individual's medical history helps healthcare providers make informed decisions in emergencies.
- Residential Lease Agreement: A critical document for rental arrangements, defining terms and protecting the rights of both landlords and tenants. For more information, visit https://floridaforms.net/blank-residential-lease-agreement-form/.
- Emergency Contact Information: This document lists individuals to contact in case of a medical emergency, ensuring that loved ones are informed and involved.
Each of these documents plays a vital role in healthcare planning. Together, they help ensure that an individual's wishes are honored and that their healthcare decisions are respected during critical moments.