Fill Your Annual Physical Examination Form
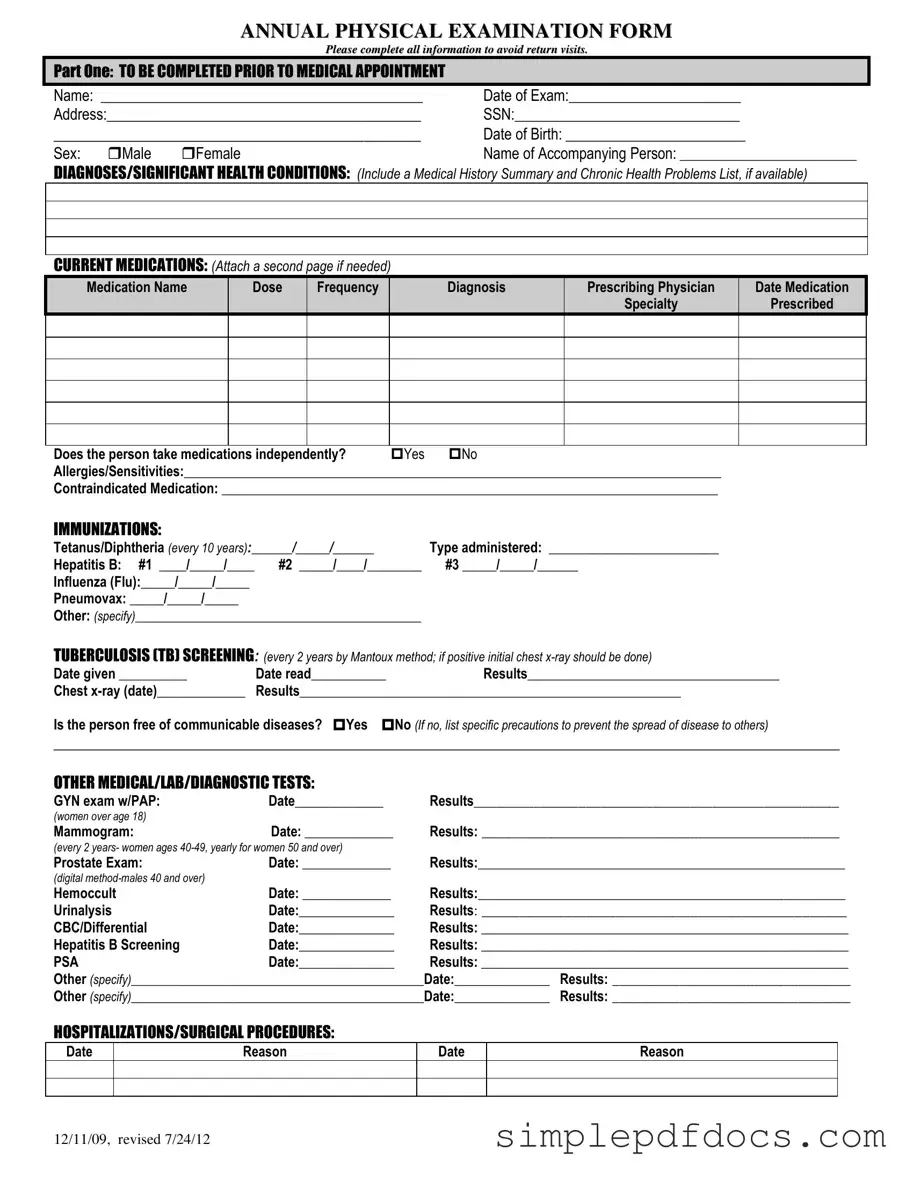
The Annual Physical Examination form is an essential tool for both patients and healthcare providers, ensuring that all necessary health information is collected before a medical appointment. This comprehensive document is divided into two main parts. The first part requires patients to provide personal details, including their name, date of birth, and medical history. It also asks for information about current medications, allergies, and immunizations, which helps the healthcare provider assess any potential risks and tailor the examination accordingly. The second part focuses on the general physical examination, where vital signs such as blood pressure and weight are recorded. Additionally, it includes an evaluation of various body systems, allowing for a thorough assessment of the individual's health. By completing this form accurately and thoroughly, patients can help minimize the need for return visits and ensure that their healthcare provider has all the information needed for a successful examination.
More PDF Templates
Act of Donation Form Louisiana - Gift transfers can impact asset distribution for future inheritances.
The Florida Divorce Settlement Agreement form is a legal document that outlines the terms and conditions agreed upon by both parties during a divorce, including important elements like asset division, child custody, and support obligations. To navigate this crucial process effectively, you may want to refer to resources such as Florida Forms, which can provide further guidance on completing the form accurately.
Texas Driver License Renewal Form - The DL-43 form is used for specific vehicle-related applications.
Document Specifics
| Fact Name | Details |
|---|---|
| Purpose | The Annual Physical Examination form is designed to gather comprehensive health information before a medical appointment. |
| Patient Information | Patients must provide personal details such as name, date of birth, and address to ensure accurate medical records. |
| Medication Disclosure | Patients are required to list current medications, including dosages and prescribing physicians, to avoid potential drug interactions. |
| Immunization Records | The form includes a section for documenting immunizations, ensuring patients are up-to-date on necessary vaccines. |
| Health History | Patients must disclose any significant health conditions and allergies, which is crucial for their overall care. |
| Screening Tests | Various screening tests are listed, such as TB screening and cancer screenings, to promote preventive health measures. |
| Legal Compliance | In many states, the completion of this form aligns with health regulations and guidelines for preventive care. |
| Recommendations | After the examination, the physician will provide recommendations for health maintenance and any necessary follow-up care. |
How to Write Annual Physical Examination
After gathering the necessary information and preparing to fill out the Annual Physical Examination form, follow these steps to ensure accurate completion. This will help streamline your medical appointment and avoid any delays.
- Begin with Part One. Fill in your Name, Date of Exam, Address, Social Security Number, and Date of Birth.
- Select your Sex by marking either the box for Male or Female.
- Provide the name of the Accompanying Person if applicable.
- List any Diagnoses or Significant Health Conditions. Include a summary of your medical history and any chronic health problems if available.
- Document your Current Medications. Include the name, dose, frequency, diagnosis, prescribing physician, and date prescribed. Attach an additional page if necessary.
- Indicate whether you take medications independently by marking Yes or No.
- List any Allergies/Sensitivities and any Contraindicated Medications.
- Fill in your Immunizations details, including dates and types administered for Tetanus/Diphtheria, Hepatitis B, Influenza, Pneumovax, and any others.
- Complete the Tuberculosis (TB) Screening section, providing the date given, date read, and results. Include chest x-ray information if applicable.
- Answer whether you are free of communicable diseases by marking Yes or No, and list any precautions if necessary.
- Document any Other Medical/Lab/Diagnostic Tests you have undergone, including dates and results for each test.
- Record any Hospitalizations/Surgical Procedures with dates and reasons.
Next, proceed to Part Two, which covers the general physical examination. This section requires vital signs and evaluations of various body systems. Ensure all information is accurately filled in to avoid any need for return visits.
- Enter your Blood Pressure, Pulse, Respirations, Temperature, Height, and Weight.
- For each system listed, indicate if the findings are normal by marking Yes or No. Provide comments or descriptions where necessary.
- Complete the Vision Screening and Hearing Screening sections, noting if further evaluation is recommended.
- Fill in the Additional Comments section, including whether your medical history summary was reviewed and any medication changes.
- Provide recommendations for health maintenance, manual exams, diet, and emergency information as needed.
- Note any limitations or restrictions for activities, including whether you use adaptive equipment.
- Indicate if there has been a change in health status from the previous year.
- Complete the final sections regarding specialty consults and seizure disorder details if applicable.
- Finally, print your physician’s name, sign, and date the form, along with providing the physician's address and phone number.
Dos and Don'ts
Things to Do:
- Complete all sections of the form to prevent delays.
- Provide accurate personal information, including your name and date of birth.
- List all current medications, including dosage and frequency.
- Include any allergies or sensitivities to medications.
- Document any significant health conditions or medical history.
- Sign and date the form before submitting it to the physician.
Things Not to Do:
- Do not leave any required fields blank.
- Avoid using abbreviations that may cause confusion.
- Do not forget to bring any necessary documents, such as previous medical records.
- Refrain from providing outdated information about medications or health conditions.
- Do not skip the immunization history section.
- Never submit the form without reviewing it for accuracy.
Documents used along the form
The Annual Physical Examination form is just one piece of the puzzle when it comes to ensuring comprehensive healthcare. Several other forms and documents often accompany it, each serving a specific purpose in the patient care process. Below is a list of commonly used forms that help to provide a fuller picture of a patient's health and medical history.
- Medical History Form: This document collects detailed information about a patient's past illnesses, surgeries, and family medical history. It helps healthcare providers understand potential hereditary conditions and previous health issues that could affect current care.
- Consent for Treatment Form: Patients sign this form to give healthcare providers permission to administer treatment or perform procedures. It ensures that patients are informed about the risks and benefits associated with their care.
- Immunization Record: This form tracks a patient’s vaccination history, including dates and types of immunizations received. It is crucial for ensuring that patients are up-to-date on necessary vaccines, especially for school or travel requirements.
- Referral Form: When a primary care physician recommends a patient to a specialist, this form outlines the reason for the referral and any relevant medical history. It facilitates communication between different healthcare providers.
- Lab Test Requisition: This document is used to order specific laboratory tests. It includes information about the tests needed and any relevant patient details to ensure accurate results.
- Notice to Quit Form: Landlords may need to include a floridaforms.net/blank-notice-to-quit-form/ to formally inform tenants about lease violations or non-renewal of tenancy, initiating the eviction process if necessary.
- Release of Information Form: Patients use this form to authorize the sharing of their medical records with other healthcare providers or institutions. It protects patient privacy while allowing for necessary communication.
- Patient Assessment Questionnaire: This form gathers information about a patient's current health status, lifestyle choices, and any symptoms they may be experiencing. It aids in identifying areas that need attention during the examination.
- Prescription Refill Request Form: Patients fill out this form to request refills for their medications. It ensures that healthcare providers are aware of ongoing medication needs and can manage prescriptions accordingly.
- Advance Directive: This legal document allows patients to outline their preferences for medical treatment in case they become unable to communicate their wishes. It is vital for ensuring that a patient's healthcare choices are respected.
Each of these forms plays a vital role in the healthcare process, helping to ensure that patients receive appropriate and effective care. Together, they create a comprehensive framework that supports both patients and healthcare providers in achieving the best health outcomes.