Fill Your Advance Beneficiary Notice of Non-coverage Form
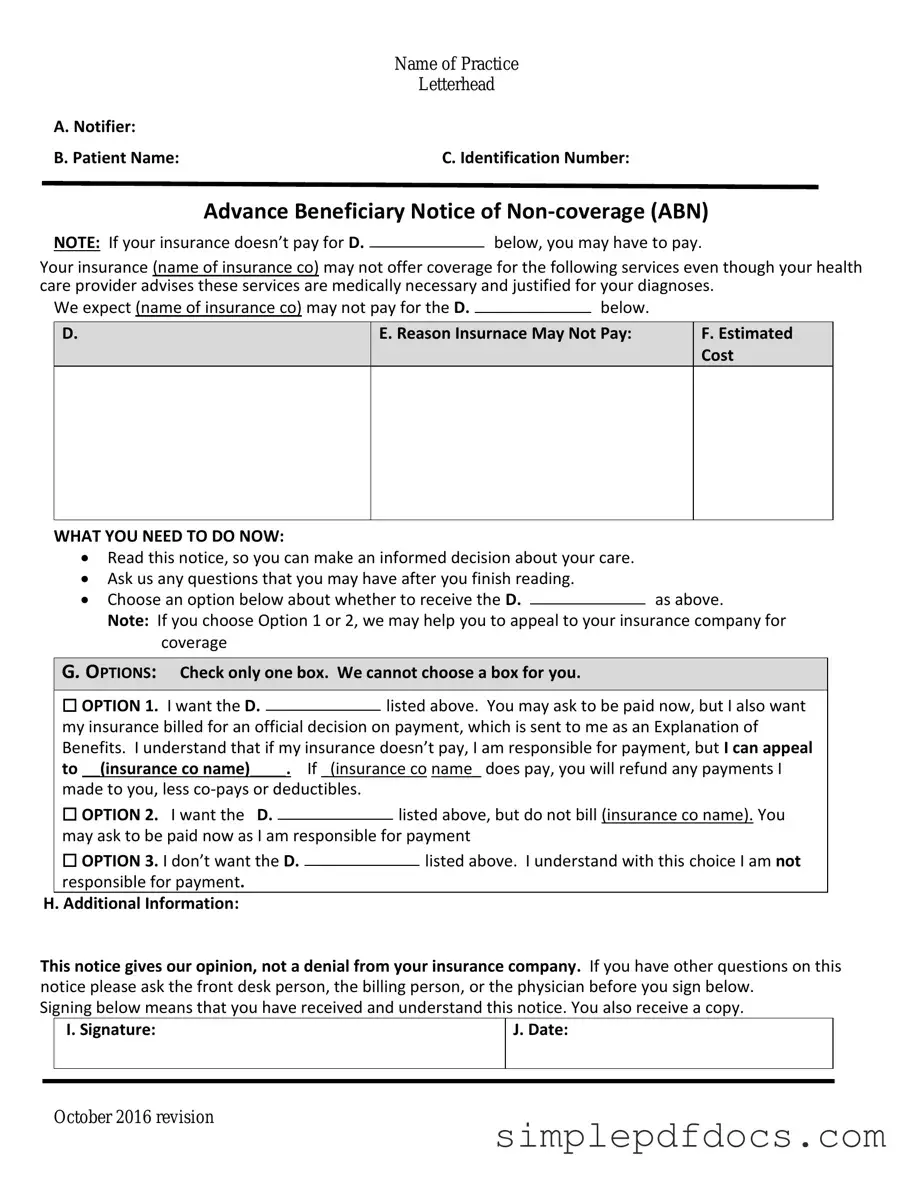
The Advance Beneficiary Notice of Non-coverage (ABN) is a critical document for Medicare beneficiaries, serving as a safeguard that ensures individuals are informed about their potential financial responsibilities for services that may not be covered by Medicare. This form is issued by healthcare providers when they believe that a particular service or item may not meet Medicare's coverage criteria. By signing the ABN, patients acknowledge that they understand the risks of receiving the service and accept that they may have to pay out of pocket if Medicare denies coverage. The ABN also outlines the specific services in question, providing clarity on why the provider believes coverage may be denied. This proactive communication allows beneficiaries to make informed decisions about their healthcare options while also protecting providers from billing disputes. Understanding the ABN is essential for anyone navigating the complexities of Medicare, as it plays a vital role in the financial planning of medical care and services.
More PDF Templates
I983 - The I-983 can also be a tool for employers to understand the educational value of training.
For individuals in Florida needing assistance with vehicle transactions, the Florida Vehicle POA form 82053 serves as a crucial tool that empowers another person to act on their behalf. This ensures that all processes, including buying, selling, or registering a vehicle, can be managed without any issues. For more information and to access the necessary documentation, you can visit Florida Forms.
2b Mindset Tracker Spiral - Create a positive mindset through daily affirmations.
Cair2 Login - Immediate access to this record can aid in unexpected health situations.
Document Specifics
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs patients that Medicare may not cover a specific service or item. |
| When to Use | Providers must issue an ABN when they believe that Medicare may deny payment for a service or item. |
| Patient Rights | Patients have the right to refuse the service after receiving the ABN, but they may be responsible for payment if Medicare denies coverage. |
| Signature Requirement | The patient must sign the ABN to acknowledge understanding of the potential non-coverage before receiving the service. |
| State-Specific Forms | Some states may have specific ABN forms governed by state laws. Check local regulations for compliance. |
| Validity Period | The ABN is valid for the specific service or item listed and is not a blanket authorization for all future services. |
| Impact on Billing | If a service is not covered, the provider can bill the patient directly for the service, provided the ABN was properly executed. |
How to Write Advance Beneficiary Notice of Non-coverage
When you receive a service that Medicare may not cover, it’s important to document your understanding of the situation. The Advance Beneficiary Notice of Non-coverage (ABN) form helps clarify that you may be responsible for payment if Medicare denies coverage. Follow these steps to fill out the form correctly.
- Obtain the Form: Get a copy of the ABN form from your healthcare provider or download it from the Medicare website.
- Fill in Your Information: At the top of the form, write your name, address, and Medicare number. This information helps identify you as the patient.
- Service Description: In the section provided, describe the service or item you are receiving. Be specific about what is being done or provided.
- Reason for Non-Coverage: The healthcare provider should explain why they believe Medicare may not cover the service. This might include details about medical necessity or other relevant factors.
- Cost Estimate: If available, include an estimate of the cost for the service. This helps you understand the potential financial responsibility.
- Patient Signature: Sign and date the form to acknowledge that you understand the information provided. Your signature indicates that you accept responsibility for payment if Medicare denies coverage.
- Provider Signature: The healthcare provider should also sign and date the form, confirming that they have discussed the information with you.
Once you’ve completed the form, keep a copy for your records. This documentation can be crucial if you need to appeal a Medicare decision later. Your healthcare provider will also retain a copy for their files.
Dos and Don'ts
When filling out the Advance Beneficiary Notice of Non-coverage (ABN) form, it's essential to approach the process with care. This form is crucial for ensuring that you understand your rights and responsibilities regarding Medicare coverage. Here are some important dos and don'ts to keep in mind:
- Do read the instructions carefully before starting to fill out the form.
- Do provide accurate information about the services you received or are about to receive.
- Do ensure that the date of service is clearly indicated on the form.
- Do sign and date the form to acknowledge your understanding of the notice.
- Do keep a copy of the completed form for your records.
- Don't leave any sections of the form blank; fill in all required fields.
- Don't rush through the process; take your time to ensure accuracy.
- Don't ignore the explanation provided in the ABN; it contains important information.
- Don't hesitate to ask questions if you are unsure about any part of the form.
By following these guidelines, you can help ensure that the ABN form is filled out correctly, minimizing any potential issues with your Medicare coverage. Remember, taking the time to understand the process is beneficial for your healthcare journey.
Documents used along the form
The Advance Beneficiary Notice of Non-coverage (ABN) is an important document that informs patients when Medicare might not cover a specific service or item. Alongside the ABN, several other forms and documents often come into play, each serving a distinct purpose in the healthcare billing and claims process. Understanding these documents can help patients navigate their healthcare options more effectively.
- Medicare Claim Form (CMS-1500): This form is used by healthcare providers to bill Medicare for services rendered. It contains essential information about the patient, the provider, and the services provided.
- Medicare Summary Notice (MSN): After a claim is processed, this notice is sent to beneficiaries. It summarizes the services billed to Medicare, detailing what was covered, what was not, and any patient responsibility.
- Authorization for Release of Health Information: This document allows healthcare providers to share a patient’s medical information with other entities, such as insurance companies or other healthcare providers, facilitating smoother claims processing.
- Georgia Tractor Bill of Sale: For smooth tractor transactions, utilize the comprehensive Georgia Tractor Bill of Sale documentation to ensure all details are accurately recorded.
- Patient Consent Form: Patients often sign this form to give their consent for treatment. It may also include consent for billing procedures and the sharing of information with insurance providers.
- Notice of Privacy Practices: This document informs patients about how their medical information will be used and protected. It is crucial for understanding patient rights regarding their health data.
- Financial Responsibility Agreement: This form outlines the patient's financial obligations regarding their treatment. It clarifies what costs the patient may incur that are not covered by insurance.
- Coordination of Benefits Form: When patients have multiple insurance plans, this form helps determine which insurance is primary and which is secondary, ensuring that claims are processed correctly.
- Medicare Advantage Plan Enrollment Form: This document is used to enroll in a Medicare Advantage plan, which may offer additional benefits beyond traditional Medicare coverage.
- Appeal Form: If a claim is denied, patients can use this form to formally appeal the decision. It outlines the reasons for the appeal and provides space for additional information.
- Durable Medical Equipment (DME) Order Form: This form is used to order medical equipment that patients may need, specifying the items and justifying their medical necessity for insurance purposes.
Familiarity with these forms can empower patients to take charge of their healthcare journey. By understanding each document's role, individuals can better advocate for themselves and ensure they receive the coverage they deserve.